It’s common and understandable for parents to worry that their little one’s sleep is being affected by pain due to reflux.
Having worked with many families struggling with GERD, Acid Reflux, gastroesophageal reflux (GER) or Reflux (all names for the same condition) I know it can be stressful and confusing.
I want to provide you with clarity and some tips that will help improve sleep even with reflux.
Having said this it’s important to note that this information is not medical advice and you should always see your doctor with any medical concerns and to get a diagnosis of reflux.
What is reflux:
Reflux is when the oesophageal sphincter that separates the stomach from the esophagus is immature and doesn’t close properly. This causes the contents of the stomach including the stomach acid to spill and come back up. It can cause vomiting but is not always associated with vomit (silent reflux). This irritates the esophagus and can cause pain and discomfort in some cases. Some babies don’t experience pain at all.
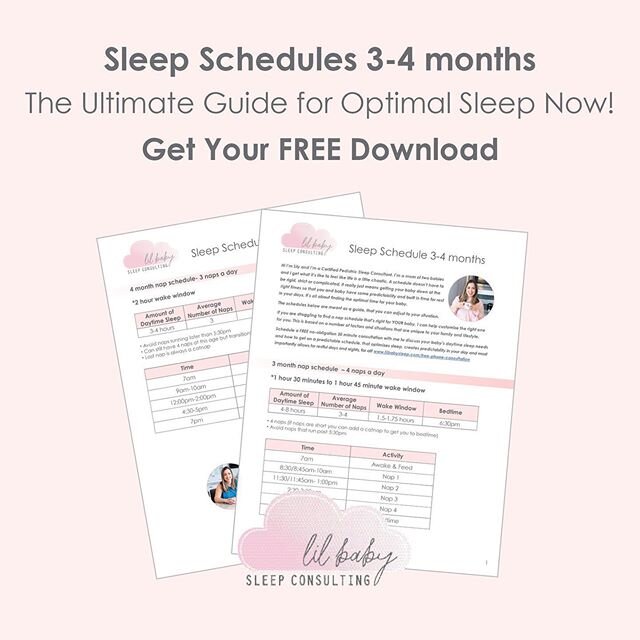
In general, most newborns experience this to a certain extent since this muscle is born immature. Spit-up is common and doesn’t always indicate reflux. Most babies will grow out of this by 3-4 months as this sphincter matures (normal spit up) but if it’s reflux it tends to last until later 4-6 months. The pain that can sometimes be associated with this can be managed with medication and a doctor can make this assessment.
Symptoms of reflux:
Spit up or vomiting
fussiness during feedings with crying (most or all feedings even during the day)
Refuses to eat
Drops in birth weight
Arching back while feeding
Wheezing, gagging, choking and hoarseness
Looking uncomfortable when lying down and arching back
Making faces looks in pain and cries
Difficulty sleeping
Why does reflux interfere with sleep?
Reflux can interfere with sleep if they are in pain or if they are taking in too much or a feed is too close to sleep. If they are in pain, laying them on their back can be uncomfortable as the acid that comes up can irritate a baby’s throat.
Also, if they are vomiting up all of their stomach contents, they could be hungry earlier.
*Remember that spit-up is common in most babies and it often seems like a lot but in reality, it looks like more than it actually is (1 oz of spit-up can look like an entire wet shirt or puddle on the floor).
Tips to help:
Paced feedings- smaller more frequent meals, taking more breaks and make sure to burp in between.
Hold upright after feeding- Holding upright and burping after feeds will help keep stomach contents down (gravity). It’s not necessary to hold for long periods of time 20-30- minutes is enough. You also don’t need to hold, you can do any activity that has them sitting upright.
If you have a newborn, pacifiers can provide some comfort following a feed you can offer a pacifier for sucking.
Separate feeds from sleep- Move your feed away from sleep so that your baby can be held upright and doesn’t fall asleep feeding. This can be done by helping them fall asleep independently (not NEEDING a feed), moving the feed to the beginning of your bedtime routine and at least 20 min before naps. This will also give them the opportunity to digest before being placed down on their backs. Many times babies who are put down right after feeding will not burp and spit up more. We can also mistake discomfort with a feed to sleep association or overtired. Speaking of…
Make sure your baby is not overtired, this is something I address in all my plans as overtired is one of the culprits behind a lot of crying in the evening hours. Work with me to ensure this is not causing your baby to have trouble sleeping.
Decrease stimulation- When a baby is overtired and over-stimulated they can become very fussy by bedtime or in the evening hours. Again, I include how to do this in every one of my sleep plans.
A few guidelines:
-Reflux will not just appear at night. It is something that you will also encounter during the day (if it’s only happening at night then I would consider working on sleep and booking a call with me).
-If your doctor has prescribed any meds they should be relieving any pain associated with reflux so we can start working on sleep!
-Many babies outgrow reflux by 6 months of age.
-Always place your baby on their back. Yes even reflux babies should be placed on their backs. The recommendation used to be to elevate the head, but that is not longer recommended as spit up while lying on their backs does not pose a threat. However, positioners, rolled blankets, pillows, wedges or anything in the crib really, do pose a risk are not safe for sleep. Also, placing babies on their tummies is a big risk of asphyxiation and positioners of positional asphixiation. The safest place is always on their backs first, if they then roll to their tummies from their backs then its okay to leave them there (as long as they rolled on their own).
Babies automatically cough up or swallow fluid that they spit up or vomit because of the gag reflex, that naturally prevents choking from happening. There is no evidence that healthy babies placed on their backs are more likely to have serious or fatal choking episodes than those placed on their stomachs. But there is strong evidence that babies placed on their stomachs are at higher risk for sudden infant death syndrome (SIDS).-American Academy of Pediatrics (AAP)
Reflux can be tough to navigate and I would argue that getting a customized sleep plan and support for a baby with reflux is so much more important. We need to make sure your babies health is considered and sleep is still possible for reflux babies. Make sure though, that you get a formal diagnosis from your doctor and see them for any pain and discomfort your baby might have. Then come to me and we can talk about how to get your baby sleeping better.
Book a free call if you are ready to get sleeping without worries, with clarity and a plan thats specific to your little one’s needs.
Lil xx
Resources:
https://www.aappublications.org/news
https://www.healthychildren.org